Lots of hubs, where are the spokes? - What the 10-Year Health Plan for England, Family Hub expansion and commitments to Local Government reform mean for babies, children and young people
7th July 2025
The end of last week saw three major policy announcements with big ambitions: the Government’s 10-year Health Plan for England, Education Secretary Bridget Philipson’s announcement of expansion of Family Hubs to every council in England, and Deputy Prime Minister Angela Rayner’s pledges on local government reform. Each is rich in rhetoric about prevention, localism, and improving outcomes for children and families.
We’re reflecting today on what this all really means for babies, children and young people and where the risks and opportunities lie.
The good news first: a shift towards local, early support
There is much to welcome in these announcements:
Health and care services are set to be decentralised, shifting more support from hospitals into communities.
The early years are rightly being prioritised, with a focus on strengthening the "Start of Life" offer (now expanded up to age five) and the expansion of Family Hubs to every council in England.
An expansion of free school meals will bring practical help to families under pressure.
Some modest but positive investment in youth mental health is being channelled into Young Futures Hubs (although emphasis on ‘modest’).
Promising action is on the horizon to tackle unhealthy food and drink marketing aimed at children, as well as other harmful influences such as vaping and other detrimental lifestyle habits.
And critically, there is repeated emphasis on prevention and early intervention, recognising that long-term health and wellbeing begins in childhood.
Certainly, these are all positive aims. However, when we look at the nuts and bolts of these reforms, there’s space to be bolder.
The substance of reforms remains reactive
Despite the language of prevention, the focus of the 10-Year Health Plan remains on treatment and reacting to problems. That’s underscored by the fact that this is where the bulk of the money will go - fixing problems after they’ve emerged rather than preventing them in the first place.
This is a familiar pattern and one we need to break to develop lasting, effective preventative approaches. And the need is more critical than ever.
The health of children and young people is getting worse
Take the 10-Year Health Plan’s bold aim: to create the “healthiest generation of children ever.” It’s a powerful aspiration, but one that rings hollow against the data. As Lord Darzi reported in 2024, children’s health is fast deteriorating. Just weeks ago, new data reported a huge increase in the proportion of young people with a common mental health disorder – rising from 19% to 26% over the last decade. This means that one in four young people now struggles with conditions like anxiety or depression that can seriously impede their potential and opportunity to thrive.
Mental health isn’t the only red flag. There are deep and growing inequities in access to and experience of health and support services, and in the outcomes of children and families from racially minoritised groups and those facing other forms of disadvantage or oppression. Poverty cuts across so many of these disparities too, and yet is barely mentioned in the 10-Year Plan.
Too many hubs, not enough spokes
There are currently a lot of local hubs planned – Family Hubs, Neighbourhood Health Centres, Youth Hubs, each housing multi-agency support teams. There is less clarity around what is really new and the relationship between the Hubs – which risks compounding the issue of duplication, rather than addressing it. Furthermore, despite the welcome injection of cash, £500m for Family Hubs pales in comparison to the £2.7 billion price tag for Sure Start, at its peak.
A missed chance for integration, or an opportunity to bridge the gap?
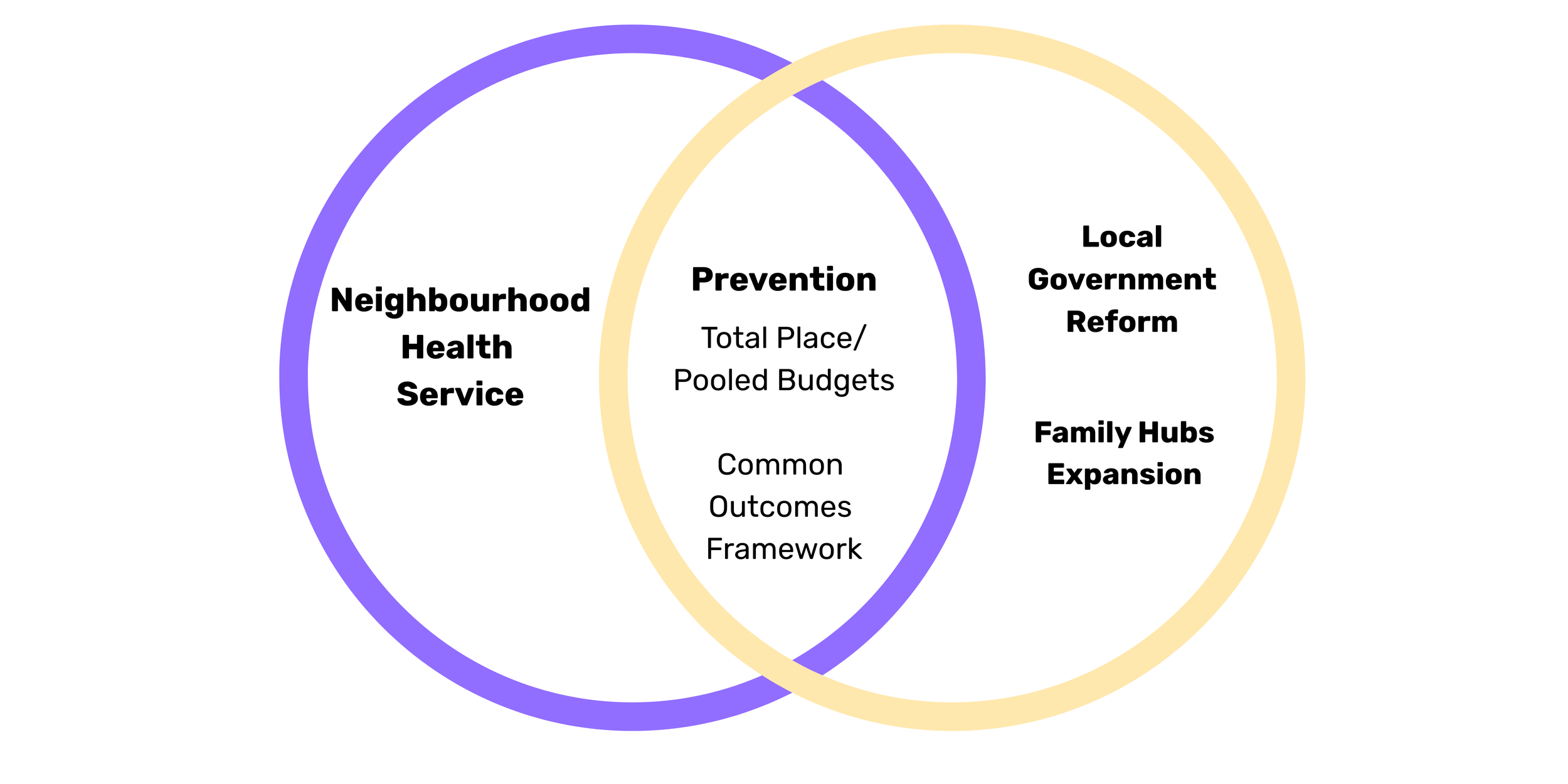
So, where is the opportunity? It is interesting to note that, despite the talk of integration and alignment, the 10-year Health Plan, Local Government reform pledges and Family Hub expansion were announced separately, over a few days and not in coordination.
Yet the real opportunity to operationalise the ideals and aspirations of each comes in how they align. The levers for prevention and the promotion of healthy child development arguably sit more within local government, public health and communities, than within the NHS, so bringing the two together is key.
Two of the Deputy Prime Minister’s announcements are of particular relevance here:
Piloting flexible funding and pooled budgets, building on the legacy of Labour’s Total Place programmes, back in 2009. This could create local mechanisms to tackle complex needs in more joined-up ways.
The development of a Local Government Outcomes Framework - a concept advocated for by our friends at the Common Outcomes for Children and Young People’s Collaborative, that we support.
Both offer practical infrastructure for integrated, community-led, and preventative approaches. Together, this is where real action, financing and co-design of community-based and coordinated preventative efforts may take shape and grow.
Where next? Turning vision into action
The vision of a healthier, fairer future for children is welcome and there is promise in the recent announcements. But the promise alone is not enough. What matters now is how these ideas are implemented and whether they genuinely shift power and investment towards communities and prevention. This will only be realised if prevention is more than a buzzword, if it is properly resourced, equitably delivered, and co-designed with the communities it’s meant to serve.
This means:
Tackling child poverty head-on.
Aligning NHS and local government efforts at both national and local levels.
Ensuring racial justice and equity are central to all reforms.
Building capacity in community-based services - especially those in early years, mental health, and family support - to think collaboratively and design and implement coordinated and holistic strategies, supported by pooled budgets and common outcomes.
It means working across silos and boundaries to reshape systems so that children and young people can thrive. That’s work that we’re passionate about driving here at Dartington. We work with communities, children and young people to design the changes they want and we support local leaders to implement those changes. We evaluate the impact of those programmes, approaches and services. And we turn evidence into practical advice to influence policy change and investment.
We think change is possible when the elements of evidence, experience and service design are considered together – this is how we drive systemic change with and for children and young people. Our current development of a Systemic Change Playbook can help shape the design and implementation of integrated Family Hub and health offers.
Our deep experience in this type of work means we’re uniquely placed to support local authorities and health services to operationalise the vision set out in these announcements. If you’re reading this and you share the ambition to build healthier, thriving futures with and for children and young people, reach out today to explore how we can work together.